While at first, they may appear the same, there are many key differences between fungal and closed comedones, including the fact that they are completely different conditions that require different treatments.
The difference between fungal acne and comedonal acne:
What is fungal acne?
Acne Vulgaris is what we typically associate as “traditional” acne. This includes blackheads, whiteheads, and inflamed zits. They are caused by clogged pores which attract C. Acnes bacteria that further inflame the condition.
Fungal acne, or more specifically, Malassezia folliculitis, presents itself as little bumps (almost like blind pimples) that don’t vary in shape or size. It is caused by an infection in the skin’s hair follicles caused by an overgrowth of yeast- Malassezia.
What causes fungal acne?
While this yeast is always present in your skin, an upset in the natural balance can lead to an overgrowth and consequently, Malassezia folliculitis. This natural balance can be thrown into disarray by a number of factors, ranging from simple things like trapped moisture from tight clothes to more complicated reasons like a suppressed immune system.
What are closed comedones?
Closed comedones are closer to "traditional acne" as we described above, in that they are caused by clogged pores from excessive sebum production and trapped skin cells. The plug of skin cells fills in the follicle swelling it up into the little bumps we know and despise.
The pore openings are obstructed by this congestion, leading the skin to have a more bumpy, swelled texture. These are different from open comedones in which the oil plug is exposed, causing them to develop a brown/black colour; these are known as blackheads.
However, closed comedones can easily develop whiteheads and when infested by P.Acnes (also known as C.Acnes) bacteria, can get inflamed leading to pustular or papular pimples.
What causes closed comedones?
Closed comedones can be attributed to the usual culprits that cause acne - pore blockage which can be caused by a number of factors including excessive oil production, dead skin cells, and trapped moisture and occlusive makeup, skincare, and haircare products. These factors depend on a number of factors including lifestyle, diet, genetics, humidity, skin type, and skincare routines.
How can you tell the difference?
Because fungal acne can look quite similar to whiteheads or blind pimples, many people try to treat it with traditional acne-targeted treatment which is usually ineffective. And vice-versa.
The first step to effectively treat any skincare condition is to effectively diagnose it. There are a number of ways you can do this. Please keep in mind that the most accurate way to diagnose your condition is for your doctor to observe your skin under a microscope.
How does it look?
Fungal acne typically looks like small red bumps, and is found in rows on the forehead and cheeks or, less commonly, on the upper back and chest.
Bacterial acne on the other hand can present itself as a whiteheads, which can be identified by a white belly.
Woodlamp examination
If you somehow have a blacklight lying around, you can CAREFULLY shine it on your skin and see what color your bumps glow. Orangey-red results mean you likely have bacterial acne. Blueish-white and yellow results mean fungus is the cause of your itchy skin.
Deductions from your environment and skin type
If you have oily skin or already prone to pimples and blackheads, there is a high likelihood that you may be also prone to comedonal acne. This makes sense because comedonal acne would definitely thrive in such an environment.
On the other hand, if you are experiencing flare ups when you are more "moist" then there is a high likelihood that the condition is fungal acne. This is because fungal acne thrives in humid, sweaty, environments and can multiply easily.
Is it possible to have both comedonal and fungal acne at the same time?
Yes, unfortunately, it is :(
Let's discuss treatment methods:
Since these are two different conditions, they require two different treatment methods.
Bacterial/Comedonal Acne
Here the goal is to minimize the congestion and stop inflammation before it begins. Traditional acne treatments like BHAs would work great to clearing pores of excessive dirt and skin cells.
Fungal Acne
If you mistake Malassezia Folliculitis for regular acne and treat it as so, however, you likely won’t get you very far. They require anti-fungal medication (usually 2% ketoconazole, econazole nitrate, or 1% clotrimazole) and sulphur-based treatments.
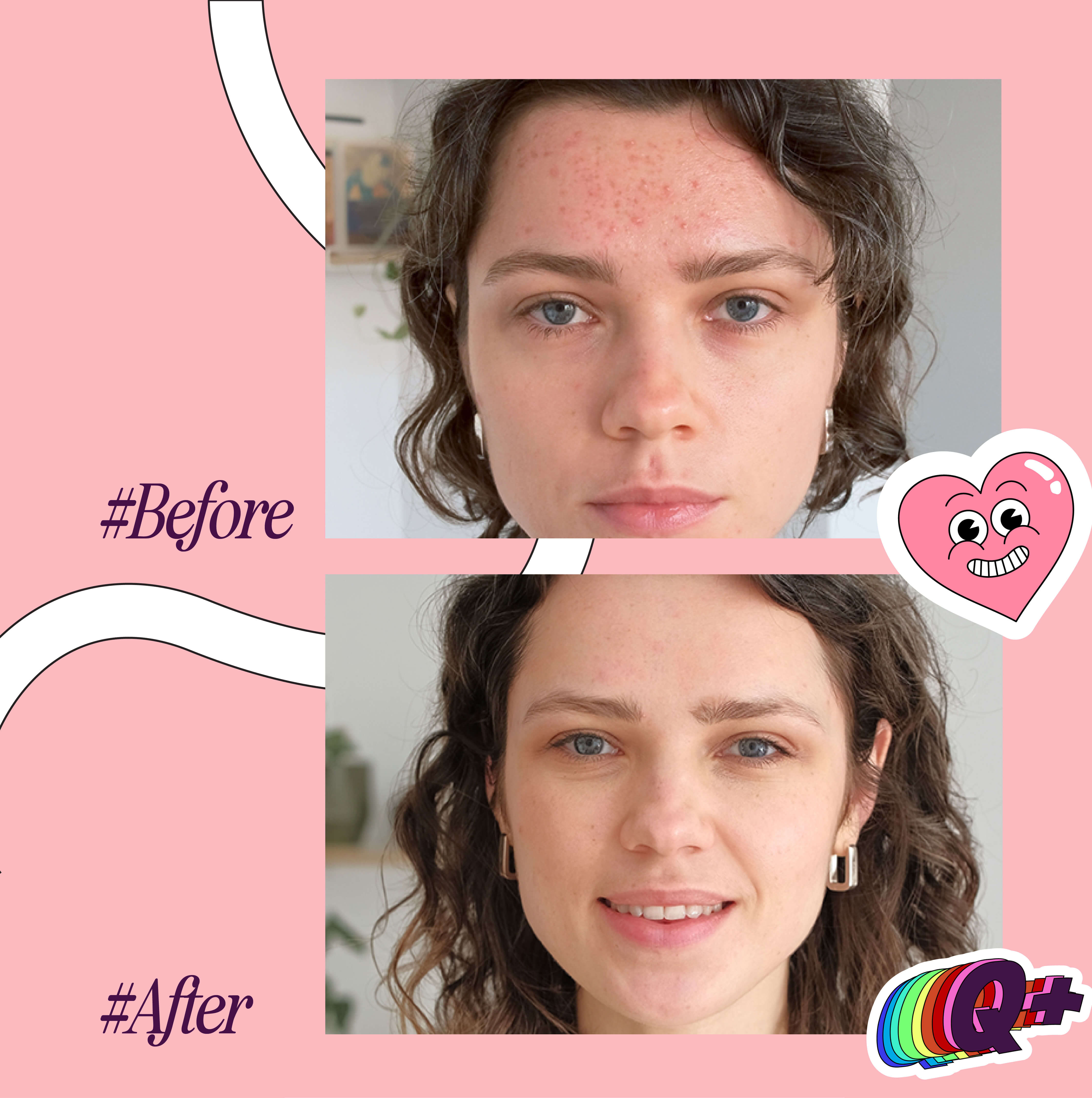
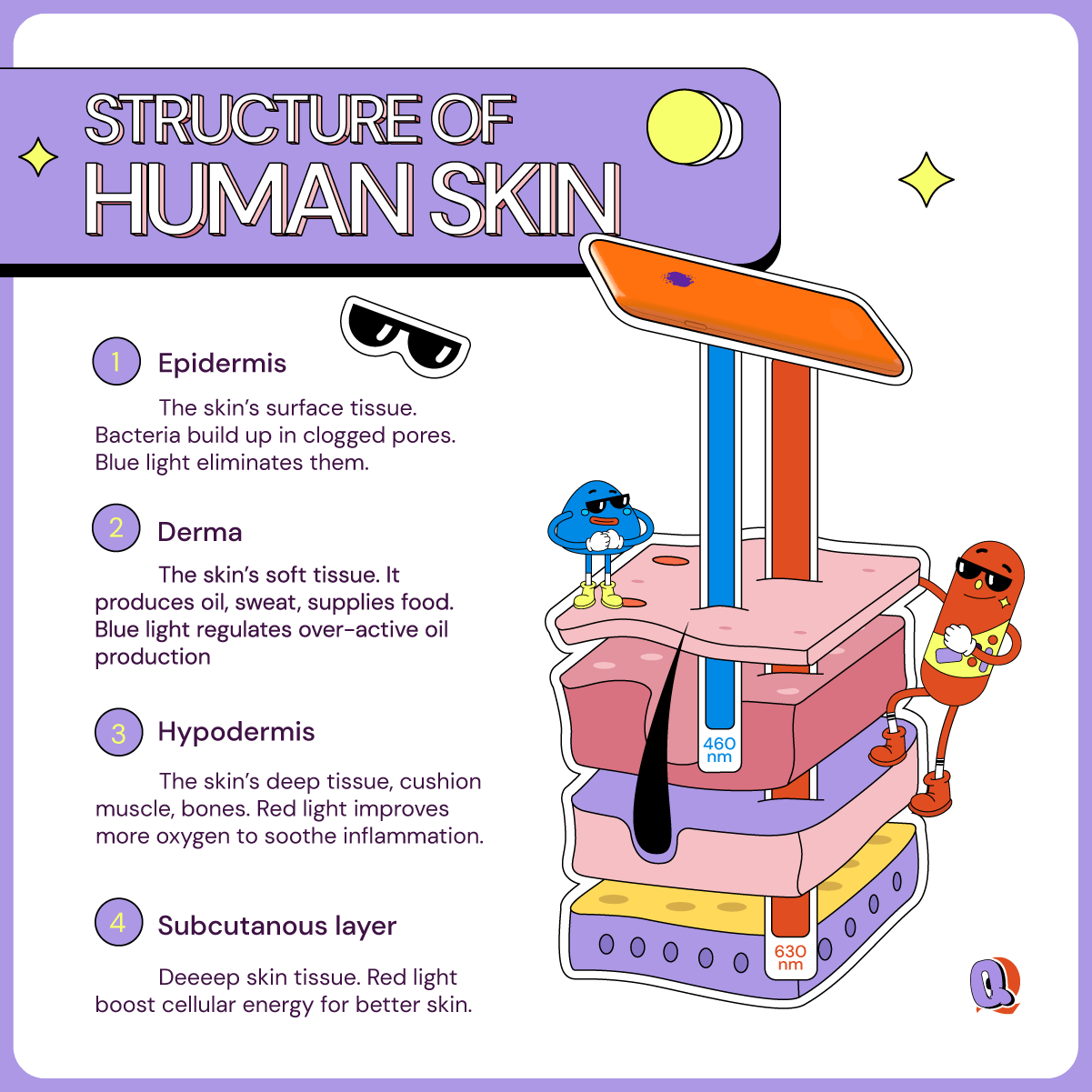
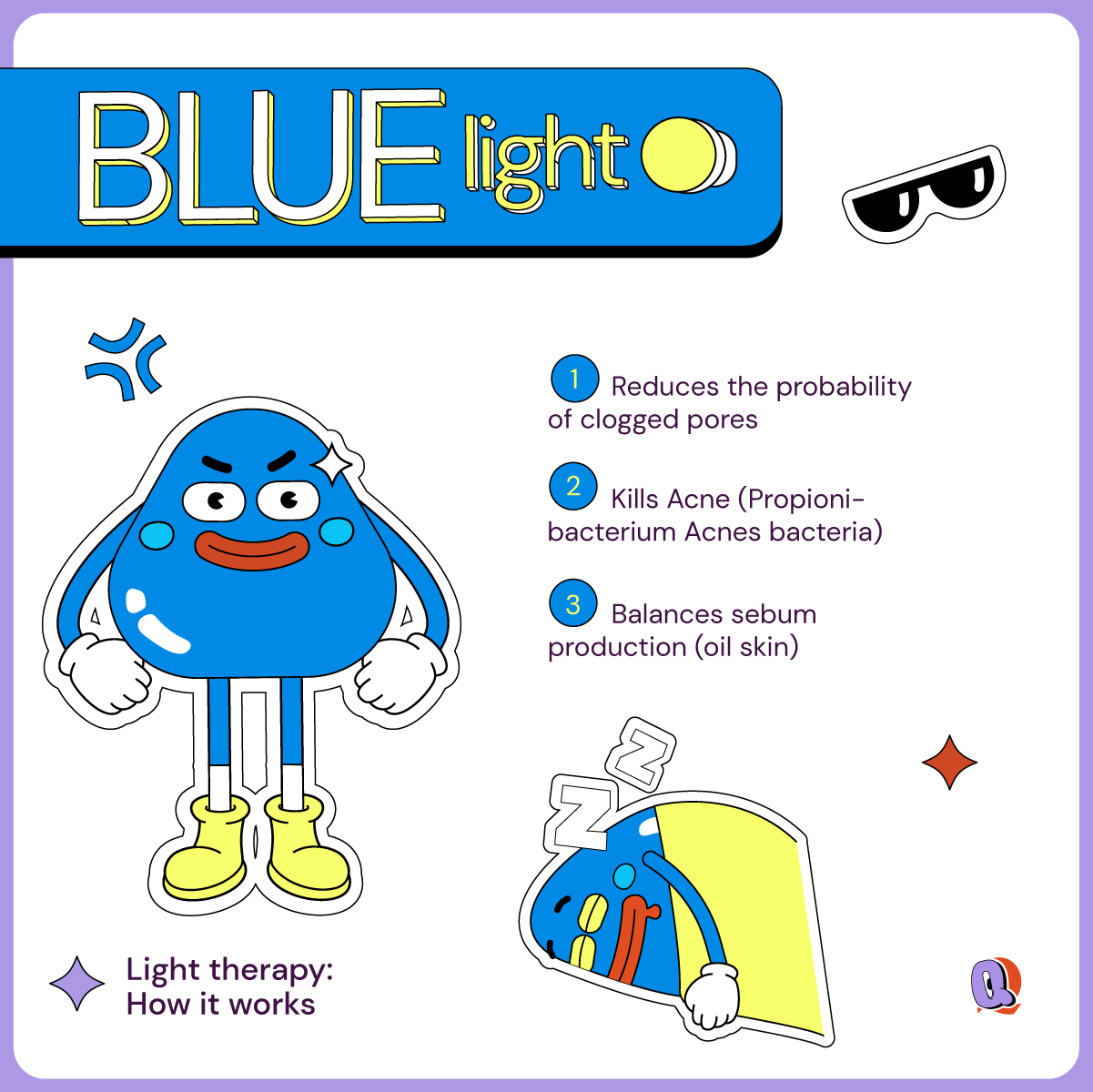
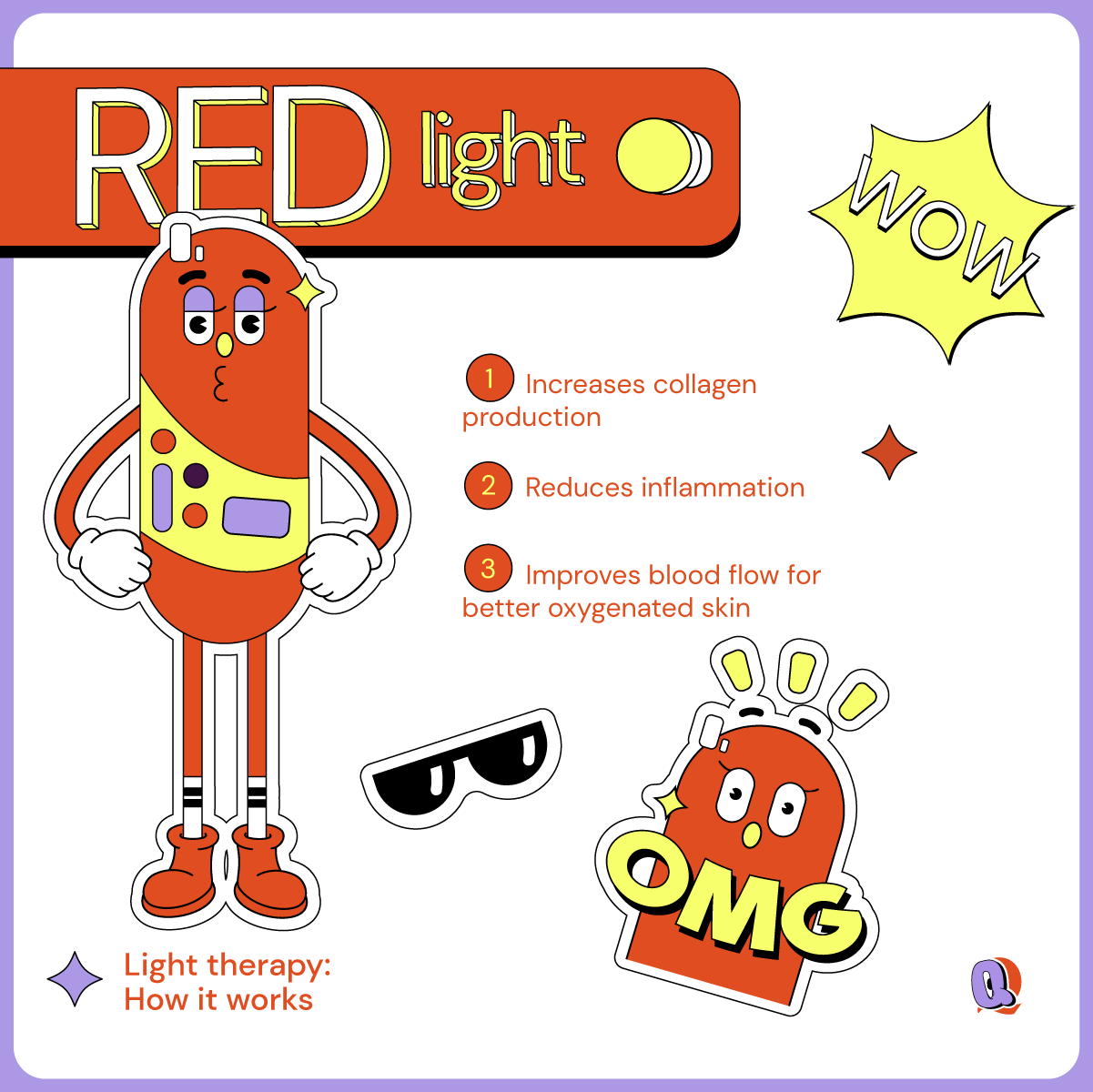
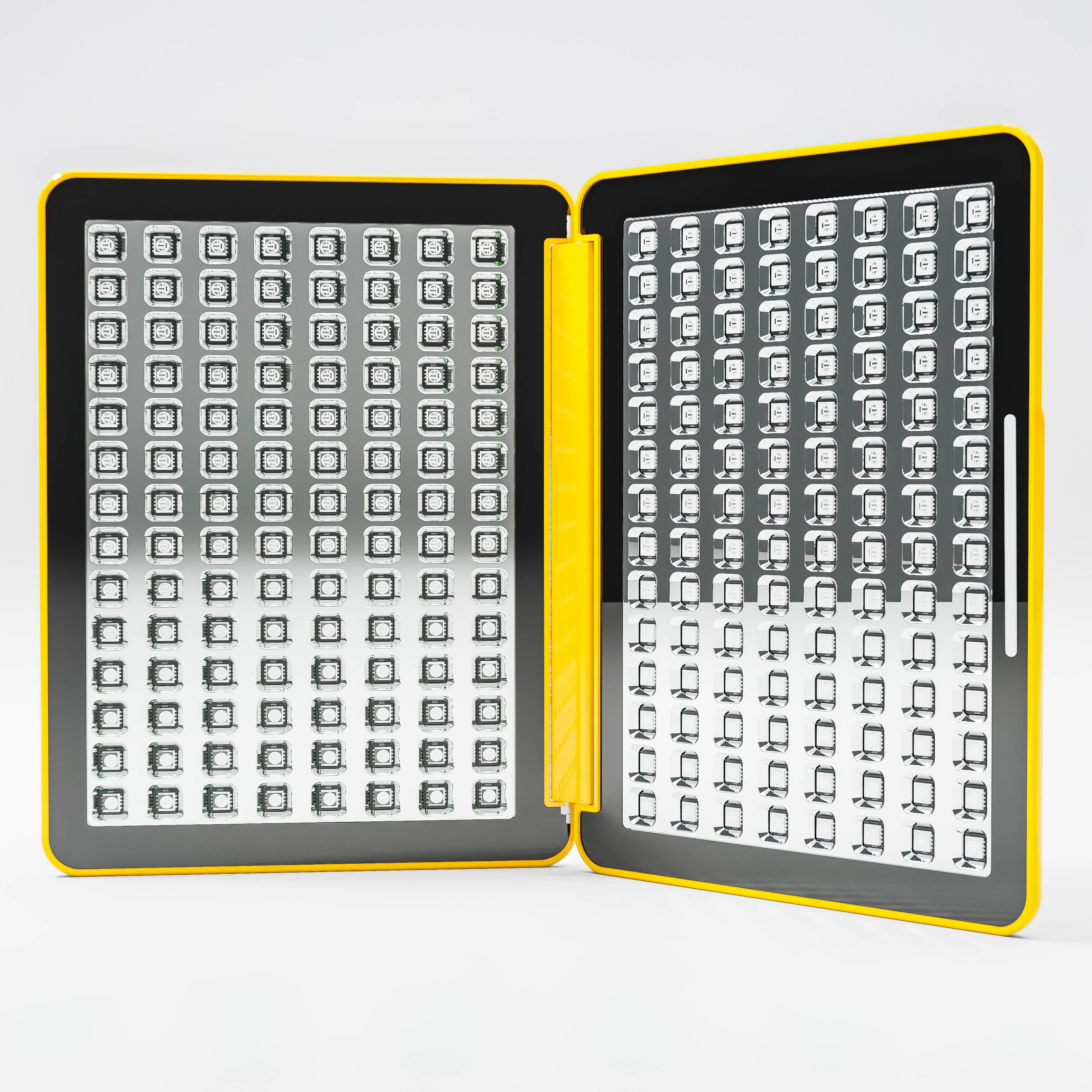
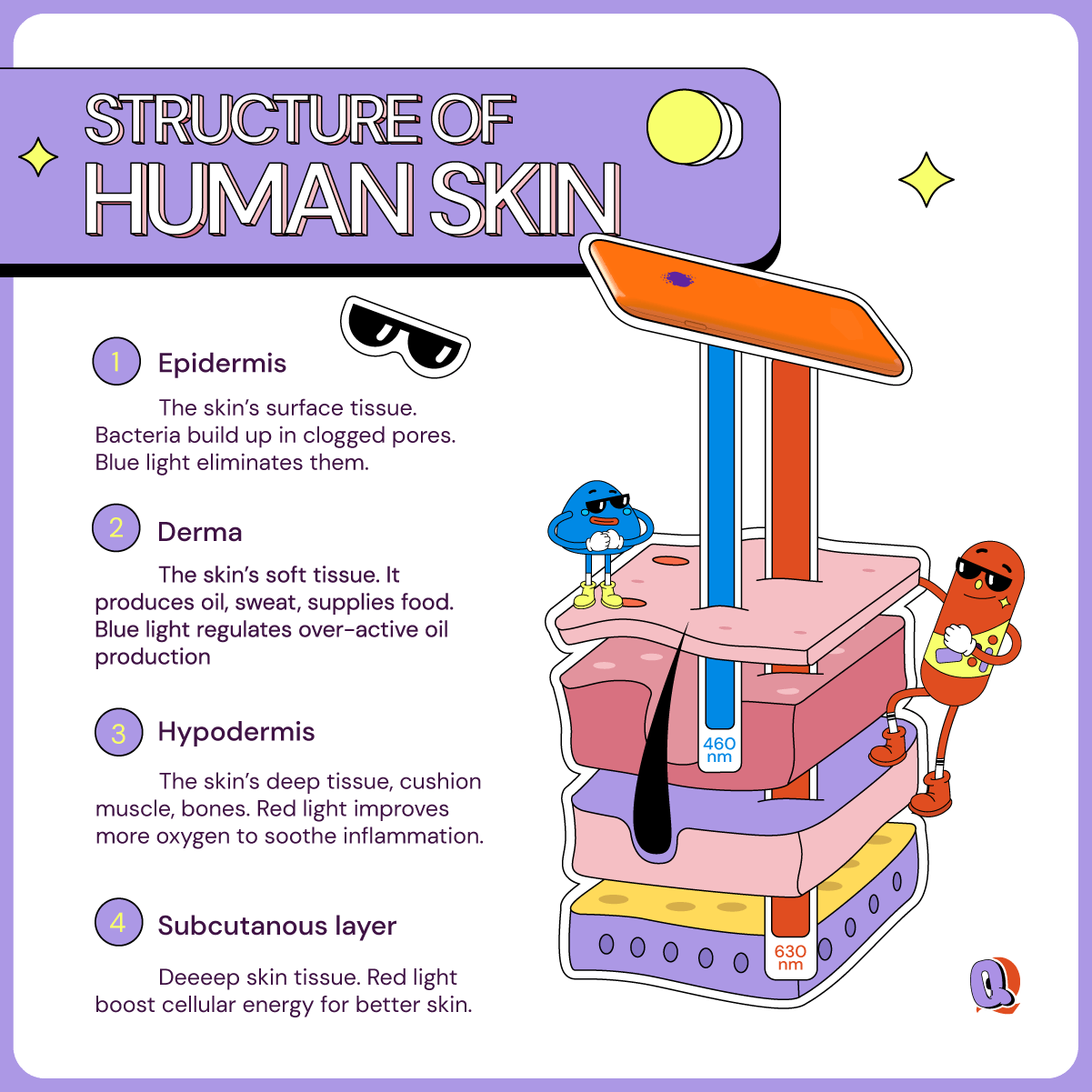
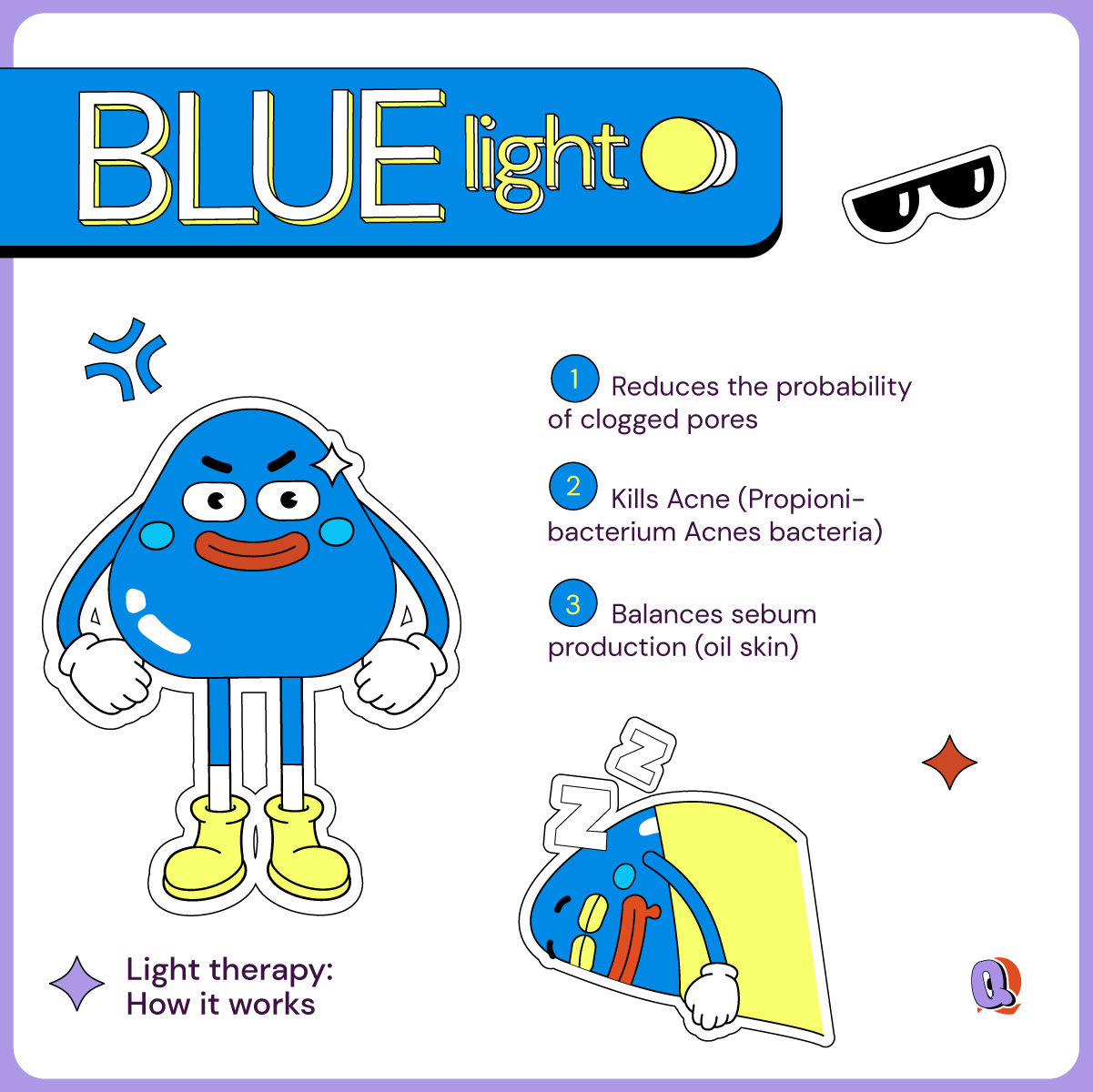
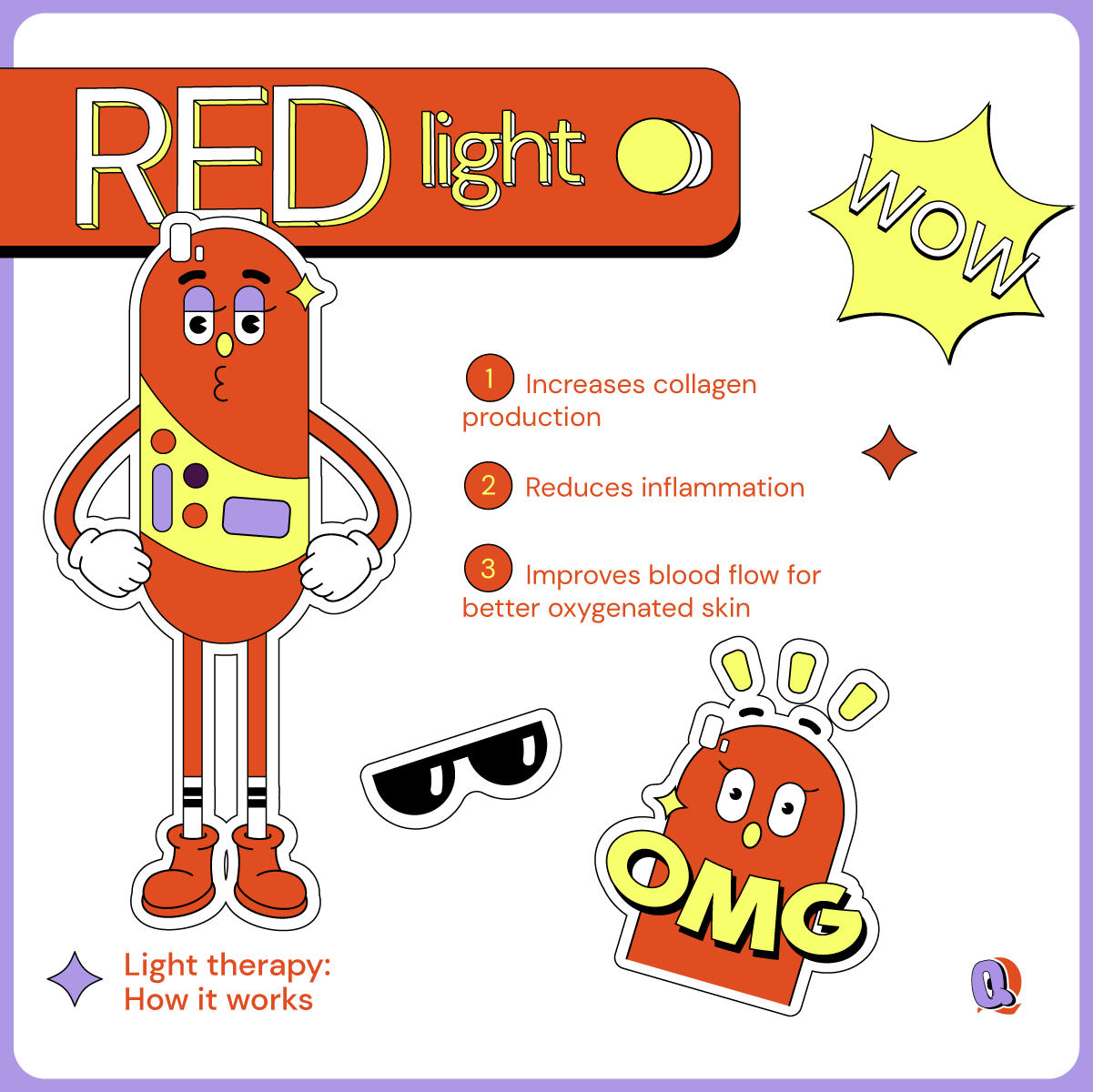
Light therapy to treat both conditions
One treatment that works both on fungal and bacterial acne is LED (Light Emitting Diode) light therapy. There is plenty of research to indicate that both P. acnes bacteria and yeast respond well to light therapy (particularly blue light therapy in this case) and can help effectively reduce and clear the skin. So, if you are going through both conditions, it’s time to give light therapy a try.